Hemorrhoids can be a painful and uncomfortable condition that many people experience at some point in their lives. These swollen veins, located inside the rectum or outside the anus, can cause pain, itching, and rectal bleeding. While hemorrhoids often resolve on their own within a few days, for some individuals, they become a chronic or recurrent problem that requires medical attention. In this article, we will explore the causes of hemorrhoids, the duration of their healing process, and various treatment options available.
Understanding the Causes of Hemorrhoids
Hemorrhoids can affect anyone, but they are commonly associated with certain factors. These include:
-
Diet low in fiber: A lack of dietary fiber can contribute to constipation, which increases the likelihood of developing hemorrhoids.
-
Weight challenges: Being overweight or obese puts extra pressure on the veins in the rectal area, making hemorrhoids more likely to occur.
-
Pregnancy: The increased pressure on the pelvic area during pregnancy can lead to the development of hemorrhoids.
-
Chronic constipation or diarrhea: Frequent straining or prolonged sitting on the toilet due to constipation or diarrhea can contribute to the formation of hemorrhoids.
-
Anal intercourse: Engaging in anal intercourse can cause irritation and swelling of the anal veins, leading to hemorrhoids.
-
Aging and muscle deterioration: As we age, the muscles in the anal and rectal areas may weaken, increasing the risk of hemorrhoids.
-
Overuse of laxatives or enemas: Excessive use of laxatives or enemas can irritate the bowel and contribute to the development of hemorrhoids.
It is essential to address the underlying causes of hemorrhoids to eliminate them effectively. For example, incorporating more fiber into your diet can improve constipation and reduce the strain during defecation, thereby reducing irritation of the anal and rectal veins and promoting healing.
The Duration of Hemorrhoid Healing
The healing time frame for hemorrhoids can vary depending on their size and severity. Smaller hemorrhoids may resolve without any treatment within a few days. However, larger external hemorrhoids may require more time to heal and can cause significant pain and discomfort in the meantime.
If your hemorrhoids do not improve within a few days or if you experience persistent symptoms, it is advisable to consult with a healthcare professional. This is especially crucial if you notice blood in your stool along with the hemorrhoids. While bright red blood is usually a result of direct irritation from hemorrhoids and will resolve when the hemorrhoids heal, darker blood may indicate a problem further up in your digestive tract and should be addressed promptly.
Promoting Hemorrhoid Healing with Lifestyle Changes
In many cases, adopting certain lifestyle habits can significantly alleviate hemorrhoid pain and promote healing. Here are some recommendations:
-
Avoid delaying bowel movements: Respond promptly to the urge to have a bowel movement to prevent constipation and reduce strain on the anal and rectal veins.
-
Use a stool for elevation: Prop your legs up on a stool while using the restroom to assume a squatting position, which can help facilitate easier bowel movements.
-
Practice good hygiene: After each bowel movement, wash the anal area with water and mild soap, or use moist wipes to keep the area clean and prevent irritation.
-
Sitz baths: Taking warm sitz baths for 10 to 15 minutes a few times a day can soothe the affected area, reduce inflammation, and promote healing.
-
Apply cold packs or ice packs: Placing cold packs or ice packs on the affected area can provide temporary relief from pain and reduce swelling.
-
Exercise regularly: Engaging in regular physical activity can help keep your bowels moving and prevent constipation, thereby reducing the risk of hemorrhoid formation.
For many individuals, over-the-counter creams or gels can effectively relieve itching and discomfort as the hemorrhoids heal. However, if these over-the-counter options are ineffective, a healthcare professional may be able to prescribe more potent topical treatments.
Medical Treatments for Persistent Hemorrhoids
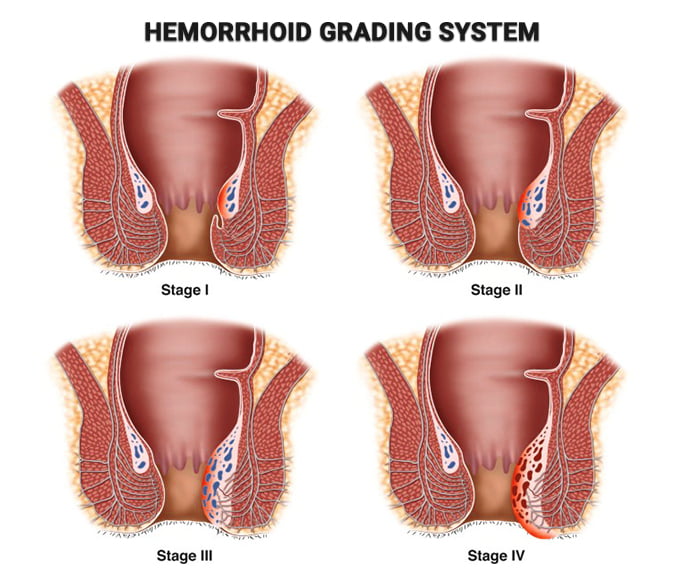
If you have persistent hemorrhoids that do not respond to lifestyle changes or if they recur frequently, more intensive medical treatments may be necessary. Some of these treatments include:
-
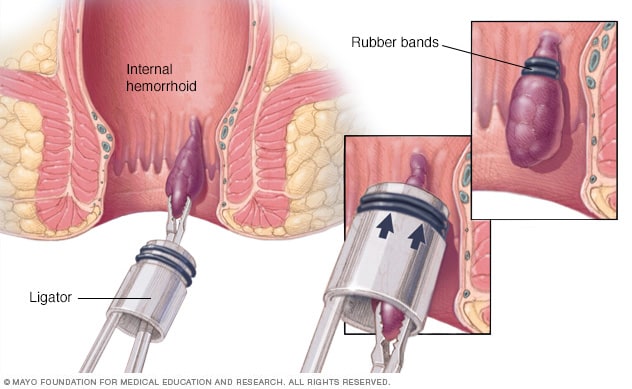
Rubber band ligation: This nonsurgical procedure involves placing a small, tight band around the base of the hemorrhoid to cut off its blood supply. As a result, the hemorrhoid shrinks and eventually falls off.
-
Sclerotherapy: In this procedure, a chemical medication is injected into the hemorrhoid, causing it to shrink and gradually disappear.
-
Surgical removal: In more severe cases, surgical removal of hemorrhoids may be necessary. This procedure is typically considered when other interventions have failed. Surgery is an effective treatment option that can prevent the recurrence of hemorrhoids.
If hemorrhoids are significantly impacting your daily life and self-care measures are not providing relief, it is crucial to seek professional medical advice. The team at Lakeland Surgical Clinic, PLLC, is dedicated to helping individuals find relief from hemorrhoid-related symptoms. They can evaluate your condition and recommend appropriate treatment options tailored to your specific needs.
In conclusion, while hemorrhoids can go away on their own within a few days, they can also become a chronic or recurrent problem for some individuals. Understanding the underlying causes of hemorrhoids and implementing lifestyle changes can promote healing and prevent their recurrence. However, if symptoms persist or worsen, medical interventions such as rubber band ligation, sclerotherapy, or surgical removal may be necessary. If you are experiencing persistent hemorrhoid-related symptoms, do not hesitate to seek medical assistance to find relief and improve your quality of life.
