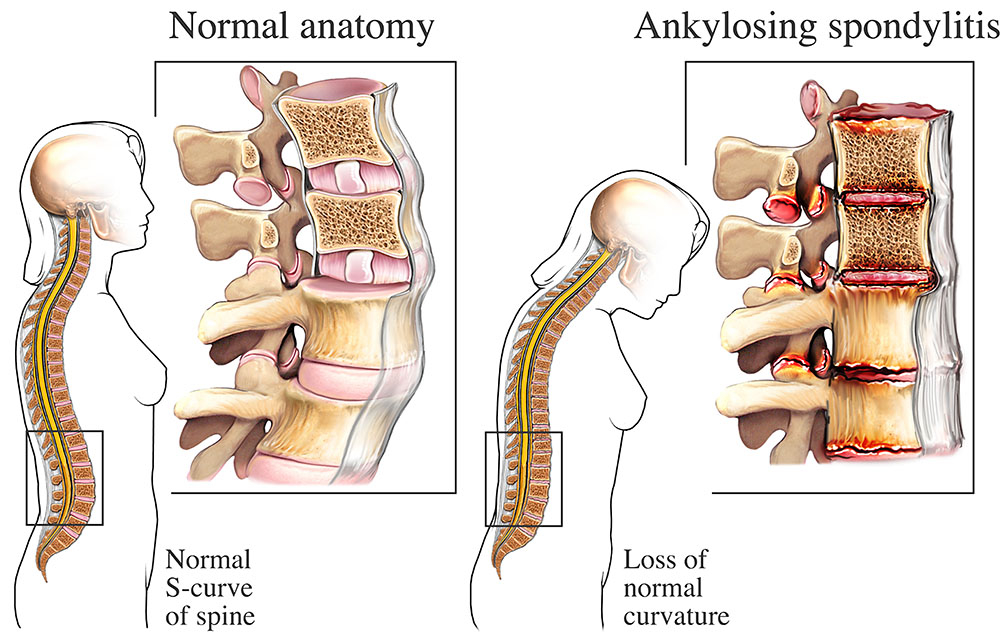
1. Overview of Ankylosing Spondylitis
Ankylosing spondylitis is a type of arthritis that primarily affects the spine. The condition is characterized by inflammation in the joints and ligaments of the spine, leading to pain, stiffness, and reduced mobility. While the exact cause of ankylosing spondylitis is unknown, researchers believe that a combination of genetic and environmental factors play a role in its development.
The symptoms of ankylosing spondylitis can vary from person to person. Some individuals may experience mild episodes of back pain and stiffness, while others may have chronic, severe pain. The pain is typically worse during periods of rest or inactivity and improves with movement and exercise. In addition to spinal symptoms, ankylosing spondylitis can also affect other areas of the body, such as the eyes, skin, and gastrointestinal tract.
2. Causes and Risk Factors
The exact cause of ankylosing spondylitis is still unknown, but researchers believe that both genetic and environmental factors contribute to its development. One of the main genetic factors associated with an increased risk of ankylosing spondylitis is the presence of the HLA-B27 gene. However, not everyone with this gene develops the condition, indicating that other factors are involved.
Other risk factors for ankylosing spondylitis include a family history of the disease, as it tends to run in families. Age is also a factor, as most people develop symptoms before the age of 45. Certain other conditions, such as Crohn’s disease, ulcerative colitis, and psoriasis, are also linked to an increased risk of developing ankylosing spondylitis.
3. Symptoms and Diagnosis
The most common symptom of ankylosing spondylitis is lower back and/or hip pain and stiffness. The pain is typically worse in the morning or after periods of rest and improves with movement and exercise. Over time, the symptoms may progress to other areas of the spine, such as the neck and upper back.
In addition to pain and stiffness, other symptoms may include inflammation in other joints, difficulty taking deep breaths, vision changes and eye pain, fatigue, loss of appetite and weight loss, skin rashes (particularly psoriasis), and abdominal pain and bowel irregularities.
To diagnose ankylosing spondylitis, healthcare professionals may perform a physical examination, review medical history, and order imaging tests such as X-rays or MRIs. Blood tests may also be conducted to check for specific markers associated with ankylosing spondylitis, such as the HLA-B27 gene.
4. Treatment Approaches
While there is no cure for ankylosing spondylitis, there are various treatment approaches available to manage symptoms and slow down disease progression. The goals of treatment are to reduce pain, stiffness, and inflammation, improve mobility and posture, and enhance overall quality of life.
The treatment plan for ankylosing spondylitis may involve a combination of medications, exercise and physical therapy, lifestyle modifications, surgical interventions, and complementary and alternative therapies. The specific approach will vary depending on the individual’s symptoms, disease severity, and response to treatment.
5. Medications for Ankylosing Spondylitis

Medications play a crucial role in managing ankylosing spondylitis symptoms and slowing down disease progression. Nonsteroidal anti-inflammatory drugs (NSAIDs) are commonly prescribed to reduce pain and inflammation. In more severe cases, biologic medications that target specific proteins involved in the inflammatory process may be used.
Corticosteroids, such as prednisone, may be prescribed for short-term symptom relief during flare-ups. Disease-modifying antirheumatic drugs (DMARDs) are sometimes used to modify the immune system’s response and slow down disease progression. It is important to work closely with a healthcare professional to determine the most appropriate medication regimen for each individual.
6. Exercise and Physical Therapy
Exercise and physical therapy are essential components of the treatment plan for ankylosing spondylitis. Regular physical activity can help improve flexibility, posture, and overall joint function. It can also reduce pain and stiffness and improve overall well-being.
Physical therapists can provide guidance on specific exercises and stretches that target the affected joints and muscles. These exercises may include stretching, strengthening, and range-of-motion exercises. It is important to work with a qualified healthcare professional to develop an exercise program tailored to individual needs and abilities.
7. Lifestyle Modifications
In addition to medications and exercise, certain lifestyle modifications can help manage ankylosing spondylitis symptoms and improve overall well-being. Maintaining good posture, using ergonomic furniture and tools, and avoiding prolonged periods of inactivity can help reduce pain and stiffness.
A healthy diet rich in anti-inflammatory foods, such as fruits, vegetables, whole grains, and lean proteins, can support overall health and reduce inflammation. Adequate rest and relaxation, stress management techniques, and getting enough sleep are also important for managing symptoms.
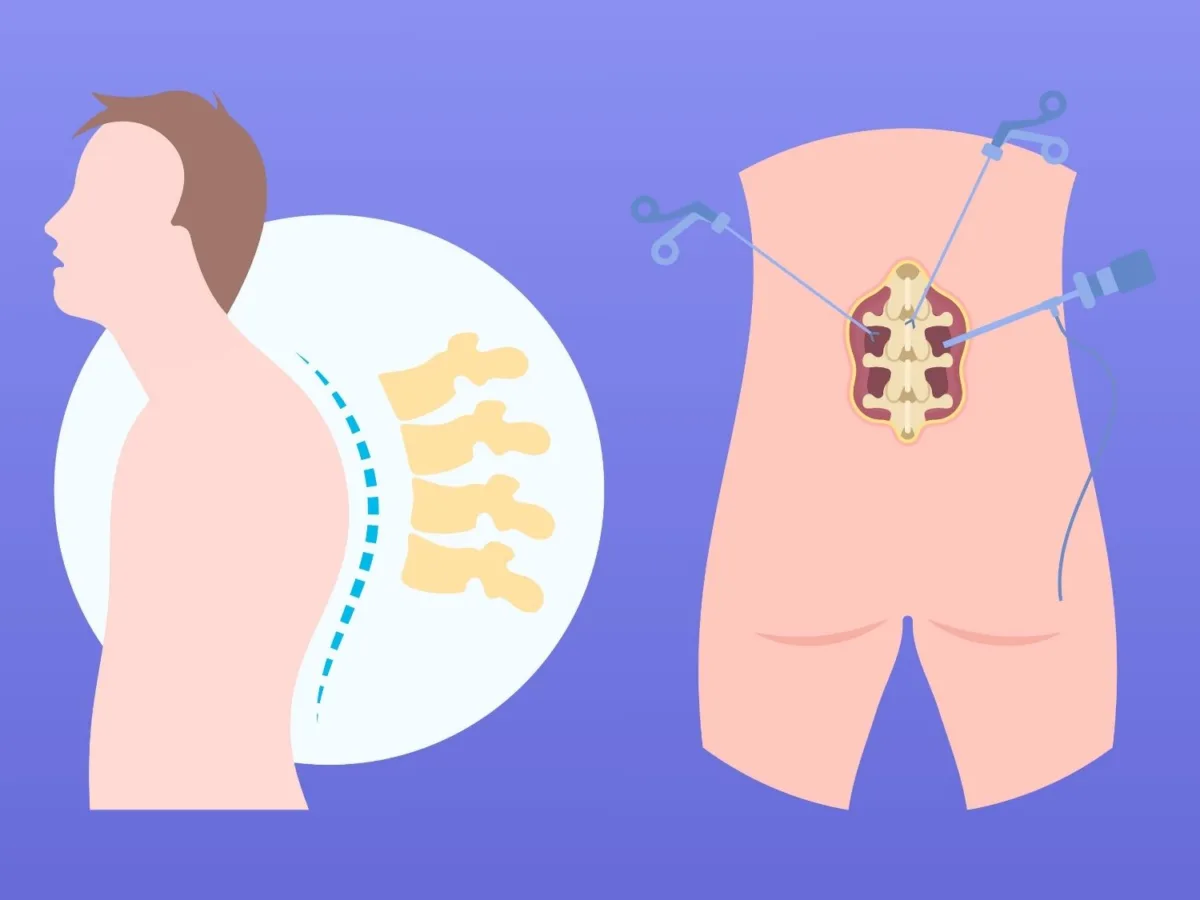
8. Surgical Interventions
Surgical interventions are generally considered a last resort for individuals with severe ankylosing spondylitis who have not responded well to other treatment options. Surgery may be recommended to correct spinal deformities, relieve pressure on the spinal cord or nerves, or replace damaged joints.
Spinal fusion surgery is the most common surgical procedure for ankylosing spondylitis. It involves fusing two or more vertebrae together to create a more stable spine. Joint replacement surgery may be considered for severely damaged hip or knee joints.
9. Complementary and Alternative Therapies
Complementary and alternative therapies can be used alongside conventional treatments to help manage ankylosing spondylitis symptoms. These therapies aim to promote relaxation, reduce pain, and improve overall well-being. Examples of complementary and alternative therapies include acupuncture, massage therapy, yoga, and meditation.
While these therapies may provide symptom relief for some individuals, it is important to consult with a healthcare professional before starting any new treatment. They can help determine the safety and effectiveness of these therapies and ensure they are used in conjunction with standard medical care.
10. Managing Flares and Preventing Complications

Ankylosing spondylitis symptoms often occur in flares, with periods of increased pain and inflammation followed by periods of relative remission. It is important to develop strategies for managing flares and preventing complications.
During flare-ups, rest, applying heat or cold packs, and taking over-the-counter pain medications may provide relief. Working closely with a healthcare professional to adjust medication dosages or try different treatment approaches can also help manage flares. It is essential to maintain regular follow-up appointments to monitor disease progression and make any necessary adjustments to the treatment plan.
11. Support and Coping Strategies
Living with ankylosing spondylitis can be challenging, both physically and emotionally. It is important to seek support from healthcare professionals, support groups, and loved ones. These resources can provide valuable information, emotional support, and coping strategies for managing the disease.
Engaging in activities that bring joy and fulfillment, practicing relaxation techniques, and maintaining a positive outlook can also help cope with the challenges of living with ankylosing spondylitis. It is important to remember that everyone’s experience with the condition is unique, and finding what works best for each individual is essential.
12. Conclusion
Ankylosing spondylitis is a chronic inflammatory condition that primarily affects the spine, causing pain, stiffness, and reduced mobility. While there is no cure, various treatment options are available to manage symptoms and improve quality of life. Medications, exercise and physical therapy, lifestyle modifications, surgical interventions, and complementary and alternative therapies can all play a role in managing ankylosing spondylitis. It is important to work closely with healthcare professionals to develop a personalized treatment plan that addresses individual needs and goals. With proper management and support, individuals with ankylosing spondylitis can lead productive and fulfilling lives.